
What is cerebrospinal fluid hypovolemia?
Cerebrospinal fluid (CSF) hypovolemia is a disease with a variety of symptoms, including headache. It occurs when cerebrospinal fluid is in a "decreased state."
[Disease Name]
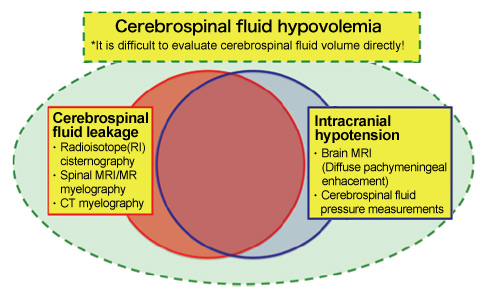
The above conceptual diagram was proposed by the study group for the establishment of a diagnosis and therapy for cerebrospinal fluid hypovolemia of the Ministry of Health, Labour and Welfare (later referred to as the Ministry of Health, Labour and Welfare (MHLW) study group).
<Intracranial Hypotension>
The medical condition characterized by severe orthostatic headache and low cerebrospinal fluid pressure (≤ 6 cm H2O), approximately corresponds to " Headache attributed to low cerebrospinal fluid pressure " as defined in the International Classification of Headache Disorders, second edition. Many of the cases are acute phase conditions. When the condition of intracranial hypotension becomes chronic, most patients eventually show mitigation of orthostatic headache and a normalization of cerebrospinal fluid pressure. We think that it is rare that acute phase conditions of intracranial hypotension continue chronically.
(Characteristics)
- Severe orthostatic headache (worsen when sitting or standing for several minutes and partially or totally regress when lying down) .
- Low cerebrospinal fluid pressure (≤ 6 cm H2O).
- Diffuse pachymeningeal enhacement, dilatation of the cerebral and epidural veins, descent or sinking or sagging of the brain, etc are often observed using brain MRI with gadolinium enhancement following the onset of symptoms.
- Conservative treatment (bed rest, fluid intake) is effective. However, cases with protracted or severe symptoms (e.g. cases with disturbance of consciousness and intracranial subdural hematomas) often require epidural blood patch therapy.
 <Cerebrospinal Fluid Leakage> Disease name proposed by the MHLW study group
<Cerebrospinal Fluid Leakage> Disease name proposed by the MHLW study group
“The core feature of cerebrospinal fluid hypovolemia is ‘cerebrospinal fluid leakage’. The MHLW study group published the diagnostic imaging criteria for cerebrospinal fluid leakage.” (2014 final study report)
From April 2016, when the definite or probable cerebrospinal fluid leakage is confirmed using this imaging criteria, we can treat the patient with epidural blood patch by adaptation of health insurance.
(Characteristics, Key Points)
- Orthostatic headache is the most common clinical manifestation. However, the degree and the interval from change in posture to the appearance of headache or relief from it are not indicated.
- The brain MRI with gadolinium enhancement findings of diffuse pachymeningeal enhancement and dilatation of intracranial veins are not included as diagnostic items. In other words, the brain MRI findings are not used for the diagnosis of cerebrospinal fluid leakage.
- Except intracranial hypotension, there will be few cases to become the diagnosis of the definite or probable cerebrospinal fluid leakage only on MRI examination. Therefore, it is necessary for patients other than those with intracranial hypotension to also perform CT myelography and RI cisternography.
<Cerebrospinal fluid hypovolemia> Disease name proposed by the cerebrospinal fluid hypovolemia study group
Clinical conditions characterized by decreases in the amount of cerebrospinal fluid include intracranial hypotension and cerebrospinal fluid leakage, as described in the above diagram. It is thought to be caused by cerebrospinal fluid leakage, a decrease in cerebrospinal fluid production, or an increase in cerebrospinal fluid absorption. Many cases of cerebrospinal fluid hypovolemia have a chronic course. We believe that RI persistence and the clearance rate of data in RI cisternography, which is not included in the imaging criteria, is very useful in disease diagnosis.
<Relationship between cerebrospinal fluid leakage and cerebrospinal fluid hypovolemia>
At present, the diagnosis of cerebrospinal fluid leakage is generally made only if there is definitive or probable spinal fluid leakage. When examining patients only with suspected symptoms or reference findings of cerebrospinal fluid leakage, there is a trend to make negative diagnosis for cerebrospinal fluid leakage and make diagnosis for different clinical conditions. In the MHLW study group, the cases only with suspected symptoms or reference findings of cerebrospinal fluid leakage are not diagnosed as negative. However, there are currently no references for the differential diagnosis of cerebrospinal fluid leakage. This highlights the need for future examination in some cases.
If we are to use imaging to diagnose patients without examining them, the presence of certain findings will indicate a diagnosis of the disease, while their absence will indicate a negative diagnosis. However, historical evidence indicates that there are many cases that have benefited from treatment, even though they were only suspected cases or showed only reference findings according to imaging findings. Therefore, we should not automatically assume that suspected cases or cases only with reference findings are manifestations of other disease states. There are also cases that have shown improvements following treatment despite a negative diagnosis based on imaging studies.
We therefore believe that cerebrospinal fluid hypovolemia must be considered as a clinical condition associated with a lesion, even if a diagnosis of cerebrospinal fluid leakage is not confirmed by imaging studies. Diagnostic imaging is effective as an objective measure. However, while the presence of cerebrospinal fluid leakage may be clearly detected by imaging in some cases, other cases may require the use of other methods or treatment options for an accurate diagnosis.
For example, we can inject saline into spinal epidural space and observe changes in the condition of the patient. This may be done by either injecting 20 to 30 ml of saline using a single puncture or by continuously injecting the solution using an epidural tube. The patient’s symptoms often show transient improvement in cases of cerebrospinal fluid hypovolemia, and there are a few patients who are cured only by the procedure of epidural saline injections.
When we treat patients shortly after the onset of symptoms, we may observe sufficient improvements and healing following “bed rest and fluid intake therapy,” which is used to treat acute intracranial hypotension. These cases are often seen in children and young people. Even if MRI examinations are conducted in such cases, it is not necessary to perform all imaging studies proposed in The MHLW study group. That would not lead to a definitive diagnosis of cerebrospinal fluid leakage in these patients. Instead, we believe that a diagnosis of cerebrospinal fluid hypovolemia can be made based on 1) the presence of specific symptoms such as orthostatic headache, 2) treatment failure for other diseases assumed or the absence of other conditions, and 3) responsiveness to bed rest and fluid intake therapy.
[Causes]
・Idiopathic: without an apparent cause, such as trauma
・Traumatic: caused by traffic accidents, sports accidents, falls, everyday bruises, violence etc.
・Iatrogenic: due to spine surgery, lumbar puncture, manipulative therapy, etc.
・Other: congenital conditions, etc.
[Etiology, Pathology]
・The etiologies of cerebrospinal fluid hypovolemia may be due to 1) cerebrospinal fluid leakage, 2) processes independent of cerbrospinal fluid leakage, such as decreases in cerebrospinal fluid production, increases in cerebrospinal fluid absorption, or spinal dural sac expansion. At present, cerbrospinal fluid leakage is considered to be the main cause of the condition.
・The symptoms of cerebrospinal fluid hypovolemia often deteriorate when the patient remains in a sitting or standing position (orthostatic exacerbation). It is thought that the amount of cerebrospinal fluid leakage increases and intracranial cerebrospinal fluid volume decreases when the body is in a raised position. This is because cerebrospinal fluid moves from the skull into the spinal canal when the body is upright.
・Brain and spinal cord exist in cerebrospinal fluid, which bathes connected structures, such as cranial nerves, spinal nerves, and blood vessels. When the volume of cerebrospinal fluid is reduced, the buoyancy effect of cerebrospinal fluid is reduced and the cranial nerves, blood vessels, and spinal nerves connected to the brain and the spinal cord are displaced downward. This leads to the appearance of a variety of symptoms, including headaches.
・It is guessed that chronic decreases in cerebrospinal fluid volume lead to secondary and tertiary symptoms, such as general fatigue, autonomic dysfunction and higher brain dysfunction.
Chronic cases of the disease often cannot be improved in a short period, even if cerebrospinal fluid leakage is treated. There may in fact be irreversible pathology in some cases.
[Symptoms]
・Among the main symptoms of the acute phase of the disease, orthostatic headache is the most frequent and significant. It is often accompanied by tinnitus, neck pain, nausea, and dizziness. As the conditions become chronic, various symptoms including general fatigue and others tend to increase. When the patients feel the acute severe orthostatic headache that cannot be sitting for several minutes, the patients are more likely to have intracranial hypotension. Therefore, bed rest therapy should be initiated promptly in such cases.
・Chronic-phase symptoms
(1) Headache (mainly orthostatic) and pain symptoms, such as neck, back, and limb pain
(2) General fatigue
(3) Cranial nerve symptoms, such as dizziness, tinnitus, visual impairment (visual loss, dazzling, etc.), facial pain or discomfort, throat discomfort, and temporomandibular joint symptoms, etc.
(4) Autonomic symptoms, such as palpitations, shortness of breath, gastrointestinal symptoms (nausea, anorexia, diarrhea, etc.), body temperature dysregulation, etc.
(5) Higher brain dysfunction symptoms, such as depression, attentional deficits, and memory loss, etc.
(6) Other: sleep disorder, susceptibility to infection, endocrine-related symptoms, etc.
Among the above symptoms, the first and second are usually present in some degree. In fact, it is exceptional for a patient to have neither of these symptoms. Therefore, we believe that the absence of both the first and second groups of symptoms is indicative of a negative diagnosis. Patients thus often present with the first two symptoms, along with some of the other symptoms described above daily and for long term. However, in cases complicated by trauma or other clinical conditions, the presence of the above symptoms may be caused by conditions other than cerebrospinal fluid hypovolemia.
While this medical condition is characterized by 1) easy deterioration of the patient’s condition in the standing or sitting positions, 2) the susceptibility of the patient to changes in the weather and atmospheric pressure, and 3) the effectiveness of water intake in symptom relief, these characteristics are not always observed in all cases.
Written by
Dr. Norimitsu Nakagawa




